Section 2: Steps Explained
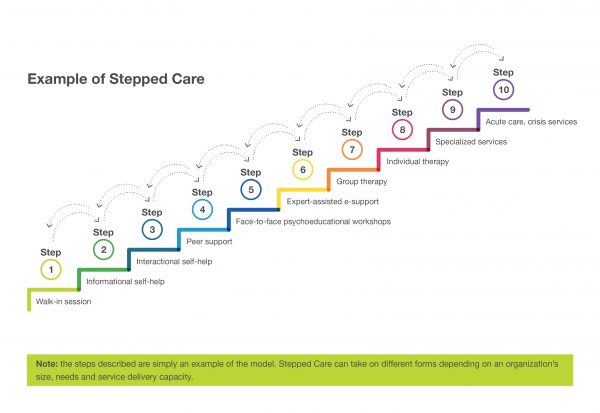
Below is an example of the detailed steps to Stepped Care 2.0 that clients may encounter depending on their intervention need. Step 1 is considered lower intensity, while Step 10 represents the most acute care. Program intensity may be stepped up or down according to where clients are on their journey.
[ Step 1 ]
First client contact: Walk-in session
Clients making a first visit are seen on a walk-in basis. This rapid access is important since early intervention is key to preventing more serious health and mental health conditions. This walk-in consultation may include an intake assessment and initial solutions-focused intervention.
By the end of the initial session, a shared plan is developed and written on a behavioural prescription form based on step level. The plan is described to clients as tentative and flexible, and they’re encouraged to make direct contact should they wish to alter the plan or miss a scheduled session. Timing and duration of a follow-up session are based on the severity of the client’s needs.
[ Step 2 ]
Informational self-help
This step involves educational self-help resources such as books, pamphlets and online media. This step aims to increase mental health literacy and engage the client in the change process when they first seek professional help.
Examples: More Feet on the Ground, JED Foundation, TED Talks, Half of Us
[ Step 3 ]
Interactional self-help
This step involves the use of interactive self-help resources, such as workbooks or courses configured for online application. These tools can be useful for students who may not be ready to fully engage in the change process, but are ready to explore what might be involved in making small changes.
Examples: WellTrack, TAO Therapy Assistance Online, Big White Wall, Good2Talk, 7 Cups
[ Step 4 ]
Peer support
This step involves the assistance of paid and/or unpaid peer workers and recovery coaches based on campus or within local community organizations. Students can benefit from the help of peer support programs, or be encouraged to become peer supporters themselves. For example, student peers can be trained by counselling staff to provide support to clients waiting at walk-in appointments or to coach e-mental health programming. Peer support can occur in-person, by phone or through online chat systems.
Examples: 7 Cups, Healthy Minds Healthy Campuses Guide, MHCC Guidelines for the Practice and Training of Peer Support, Peer Support Canada
[ Step 5 ]
Face-to-face psychoeducational workshops
This step involves interactive, psychoeducational, professionally-facilitated, skill-building workshops. A variety of peer and professionally-led online chats and face-to-face interventions are offered on a drop-in, single-session basis or through a series of coaching workshops.
Examples: SMART Recovery, stress management, Canadian Mental Health Association workshops
[ Step 6 ]
Expert-assisted e-support
This step involves therapist-assisted online mental health programming. Clients enrolled in therapist-assisted e-mental health programs are typically assigned to a provider who spends 15-20 minutes per week providing online or telephone coaching and support as participants work through care modules. Outcome monitoring is built into these programs.
Examples: BounceBack, TAO Therapist Assistance Online, keep.meSAFE, Sanvello
[ Step 7 ]
Group therapy
This step involves intensive group programming and/or training sessions that are professionally led, and participating clients are initially referred by a clinician. Please note that this step is lower than Step 8 in terms of cost, but may be higher in terms of intensity and client readiness.
Examples: Group programs related to mindfulness, depression, anxiety, cognitive behavioural therapy (CBT)
[ Step 8 ]
Individual therapy
This step involves more intensive one-on-one counselling sessions. Individual therapy is intense work during which clients are asked to set clear goals and work towards these with therapist guidance. Counsellors are encouraged to use time creatively and with some flexibility. Some clients with severe symptoms are seen weekly for sessions ranging from 20-50 minutes. Others are seen for brief check-ins on a bi-weekly basis. Clients who are in the recovery or maintenance stage may be seen only every three or four weeks with self-help resources assigned as homework.
Examples: Evidence-informed face-to-face counselling which includes but is not limited to CBT, dialectical behaviour therapy (DBT), interpersonal and brief psychodynamic therapy.
[ Step 9 ]
Specialized services
This step involves outpatient psychiatric consultation for individuals that don’t show progress at Step 8 and/or specialized community-based services for clients with chronic mental health conditions that require long-term or prolonged intensive treatment.
Examples: Canadian Mental Health Association services, private psychotherapy, women’s shelters, sexual assault clinics
[ Step 10 ]
Acute care, crisis services
This step involves intensive case management and crisis support for clients with chronic conditions, substance use and/or behavioural issues. This includes more intensive services such as admission to a hospital psychiatric ward.
Most Step 10 activities are co-ordinated by case managers who liaise between campus officials and community-based agencies to ensure continuity of care.
Examples: Campus safety and security, Canadian Mental Health Association crisis services, police, hospital emergency

