Lily’s Story
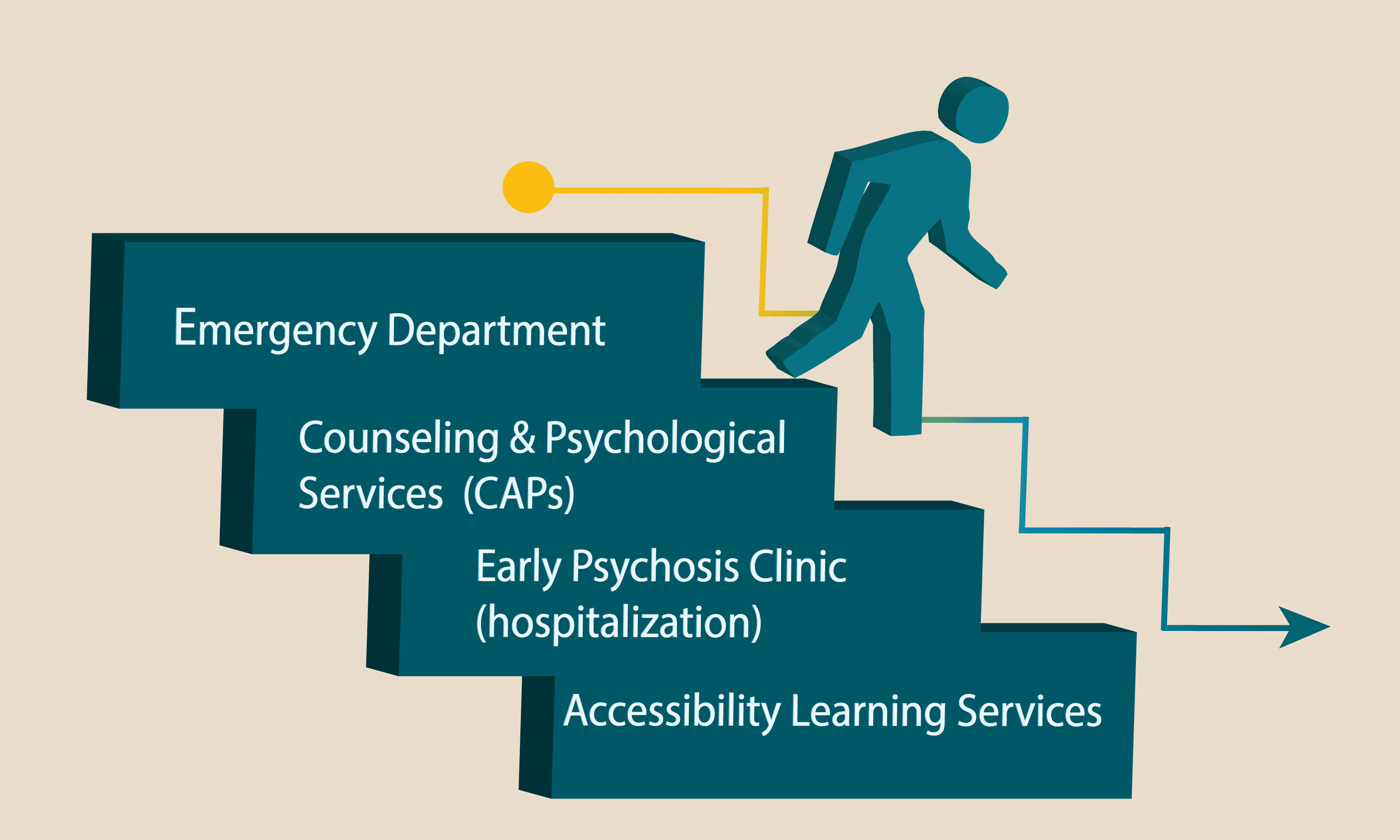
This case study highlights a pathway to the Early Psychosis Intervention (EPI) service.
Student Profile
Lily is a 19-year old student attending her 2nd year of university in her home town. Lily lives at home with her parents, is a varsity athlete and maintained good grades prior to her diagnosis.
Presenting concern
Hypomania and delusions
Background Story
Lily is a 19-year old student attending her 2nd year of university in her home town. Lily lives at home with her parents. Lily is a varsity athlete and maintains good grades. However, during the summer Lily started to experience paranoid thoughts and grandiose ideas. Lily’s mother took her to the emergency department at their local hospital where she was diagnosed with having experienced an episode of hypomania. Lily was discharged with a list of supports on her campus and registered with her university’s Counseling and Psychological Services (CAPS). While receiving services through CAPS, Lily was trialed on medication, her mood stabilized but the delusions persisted. As a result, Lily began isolating herself from her peers and family and quit playing varsity sports. Lily later decided to discontinue her medication due to the side effects; her academic performance then declined dramatically.
Due to Lily’s persistent delusions her CAPS worker thought it would be best to refer her to the local Early Psychosis Intervention (EPI) service. The CAPS worker accessed the Early Psychosis Intervention Ontario Network website (www.epion.ca) to locate a local EPI clinic. The EPI clinic provided a referral form and a Consent for Disclosure of Personal Health Information form for the CAPS worker and Lily to sign and complete (see, Sample Consent Form). The CAPS worker accompanied Lily to this appointment and provided collateral information for the 1.5 years that Lily had received services.
Upon this initial assessment, the EPI worker determined that Lily had ongoing delusions. Lily then needed to be hospitalized for approximately 2 weeks. After hospitalization, Lily worked with her EPI team which included a psychiatrist and a case manager. With Lily’s consent, her EPI case manager contacted the CAPS worker to discuss potential on-campus supports available to Lily that would assist with her transition back to school. The case manager and Lily’s psychiatrist discussed connecting Lily with Accessibility Learning Services (ALS) at the university, to which Lily agreed. Lily’s case manager and psychiatrist prepared a letter outlining that Lily could experience academic difficulties as a result of her symptoms and medications and may require academic accommodations (see, Sample Accessibility Learning Service Letter). Lily signed a consent form that allowed her treatment team to talk with ALS regarding these potential helpful accommodations.
Throughout Lily’s recovery, she had difficulty focusing on classroom material due to memory problems. Lily found her ALS counselor supportive and helpful in recommending specific accommodations that would promote successful academic performance; however she had great difficulty with these accommodations being accepted by all of her professors.
With the ongoing support of Lily’s EPI treatment team and ALS she completed her degree in five and a half years.
First Point of Contact
Lily’s first point of contact was her local emergency department.
Carepath
Treatment Plan
- EPI Clinic
- Specialized assessment e.g. cognitive, neuropsychological
- Intensive case management
- Medical treatment – medication management, physical health monitoring
- Psychosis education
- Provides family support
- Psychosocial rehabilitation – CBT for psychosis, stress management, social supports and skills, relapse prevention, life skills
- Concurrent disorder work
- Involve intervention for a period that ranges from 1-3 years
- Focuses on the principles of hope and recovery
- Accessibility Learning Services
- Liaise with EPI team regarding client’s cognitive abilities that are influenced by psychosis as well as medication, access to neuropsychological test results if available
- Provide accommodation recommendations based on client’s abilities and assist with advocating for these accommodations in lectures
- CAPS:
- Ongoing individual support, as indicated and desired by client
- Ongoing discussions regarding available on-campus supports that might be valuable e.g. peer support services, study skills services
Key Considerations
- Consent – have the student sign a consent form that allows for communication with their treating team; explain the benefits of this open communication to better serve all of the student’s needs e.g. academic, medical, social, etc; circle of care concept.
- Often when a client/student goes to the emergency room, they are provided with follow up recommendations; however due to the nature of emergency services, ensuring this linkage is not always possible and therefore it is relied upon the client and/or family to do so.
- Accompany the student to their medical appointment, to provide collateral and to promote the building of partnerships with the treatment team – with the student’s consent only
- The EPI team likely does not have a full understanding of all the available on-campus supports, therefore having regular conversations with the treatment team is valuable
- Collaboration is key – it is the best way to ensure that a student’s/client’s needs are best met – the EPI team WANTS to collaborate
- EPI services can be accessed and initiated by various referral sources – including on-campus supports; go to http://epion.ca/looking-for-help/where-to-get-help for the contact information for every EPI service that covers every geographic area of the province
- EPI services can be contacted for consultation or to assess if a student is appropriate for their services – if the on-campus supports are not sure
- Family support of the student is usually key; sometimes it is helpful to hear the family’s perspective and this can be done with the student’s consent; the family can be part of the intervention and circle of care; however not all students want their family involved. EPI services are family sensitive and work with the client to include the family in their recovery; sometimes family support can be helpful to assist with the follow through of treatment recommendations and sometimes families require support themselves and education on how to support their loved one – often EPI services have a family support worker as part of their team or have access to family support services. Independent of the family support services connected with an EPI team; there are usually community family support services available.
- Each student’s experience with psychosis is different and their needs will be different – medically, academically, socially
- Engagement is key
- Recovery and hope are important principles
- Psychosis is treatable and does not define the individual
Additional Information
EPI Objectives
- Minimize the duration of untreated psychosis (DUP) – improves outcomes and treatment resistance
- Minimize disruption of roles and responsibilities, relationships, and social skills
- Minimize substance use and other co-morbidities
- Minimize safety risks & hospitalizations
Key Elements of an EPI Progam (MOHLTC)
- Early identification, facilitating access
- Comprehensive assessment
- Treatment – intensive follow up; appropriate and individualized treatment (medical – diagnostic assessment, medication assessment, metabolic interventions; and case management – see psychosocial support)
- Psychosocial support (coping strategies & independent living skills, educational/academic, vocational/employment, housing, social/recreational, peer support)
- Family education and support
- Normalized recovery context
- Education and research