Home Stepped Care 2.0 Toolkit Section 3: Case Studies The Case of the University of Toronto
The Case of the University of Toronto
Background
Prior to fall 2015, Health and Wellness consisted of two distinct clinics, Health Services (HS) and Counselling & Psychological Services (CAPS). In September 2015, the two clinics were integrated into the Health & Wellness Centre (HWC) to provide an interdisciplinary collaborative care model for students. With that, a formalized Stepped Care Model was adopted for mental health services. The integration was a direct response to the University of Toronto Mental Health Framework, student feedback, and best practices to ensure students have quicker, direct access to health and mental health services.
The Process
- Centralized intake: Students can now access all services, including family physicians, nurses, psychologists, social workers, psychiatrists, a dietitian, and support staff through one single access point. Students are assessed through one intake process and receive interdisciplinary care based on their needs.
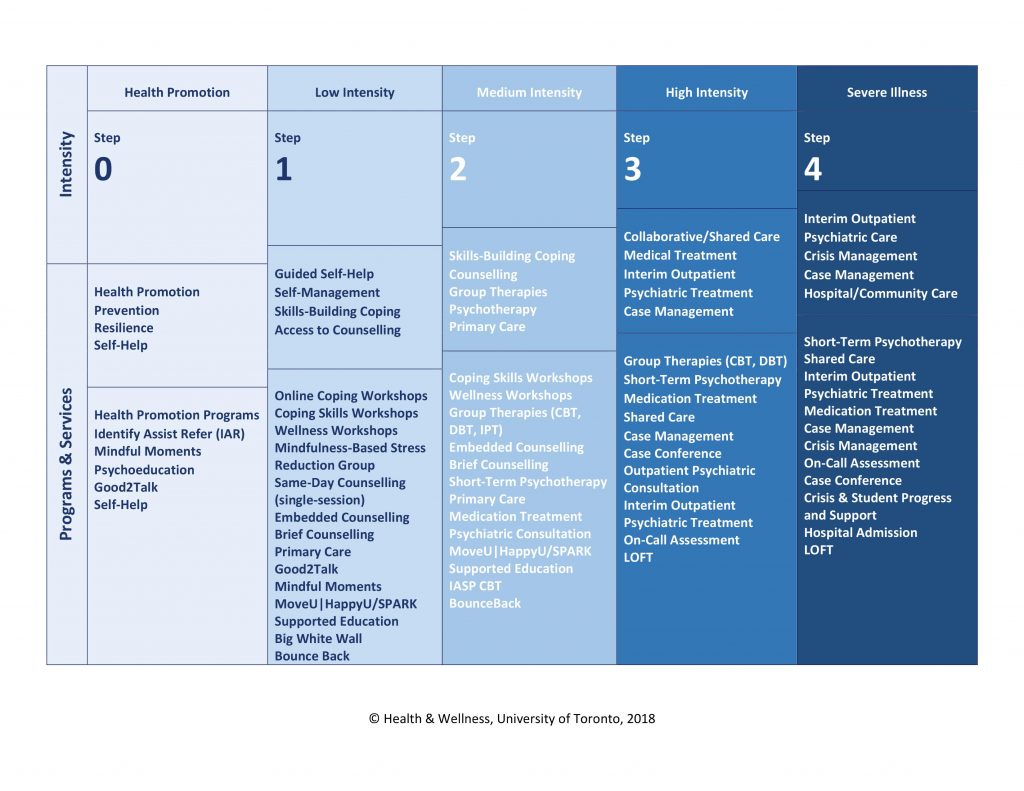
- Triage: Based on a mental health intake, students are matched to the most accessible, lowest intensity, and most autonomous mental health program, ranging from psychoeducational workshops, brief counselling, short-term group or individual psychotherapy, psychiatric care, case management, and urgent services.
- Psychoeducational workshops: A four-module, CBT-based coping skills workshop was developed in addition to wellness workshops focused on sleep and relaxation strategies. These workshops could be the recommended care pathway from triage or accessed during waits for more intensive services.
- Embedded/on-location counselling: Expansion of embedded counselling to over 20 faculties, colleges, and departments.
- Group therapy: Several evidence-based eight-week groups were developed, including a trans-diagnostic CBT group for depression and anxiety, DBT group for emotional dysregulation and low distress tolerance in the context of depression and anxiety, DBT group for personality issues with higher complexity (suicidality, self-harm), and a four-week mindfulness-based stress reduction group.
- Shared care: Psychiatrists are embedded within the medical team, providing psychiatric consultation and short episodes of care, with follow-up provided by the referring family physician.
- Shared electronic medical record (EMR): All clinicians utilize the same EMR, with one clinical chart for each student.
- Training: All clinical and administrative staff were provided with training sessions on the new model of care. Primary care physicians and nurses shadowed psychologists during mental health intakes and consulted on guidelines for determining urgency and disposition.
- Collaborative care: a. Interdisciplinary case conference teams are established each academic year. They meet monthly to discuss clinical cases.
- Interdisciplinary teams are established for specialized care (e.g., trans health care team).
- A complex care team was established to review treatment plans for students with complex needs. The team meets weekly or twice weekly and clinicians can join the meetings to discuss students of concern and treatment plans.
- Shared care consultations are hosted by a psychiatrist every afternoon for clinicians to consult on shared care cases, medication treatment, diagnostic issues, etc.
The Results
- Pathway approach: Single access point provides a more accountable, clear, and guided pathway to care.
- Centralized services reduce fractured care and duplication of services and provide an ongoing monitoring system rather than siloed care.
- Stepped Care Model matches severity of student concerns to intensity of mental health services.
- Promotes episodes of mental health care, with follow-up provided by primary care and opportunity for mental health consultation as needed.
- Promotes interdisciplinary care teams focused on specialized populations (e.g., trans health, eating disorders, trauma) and improves student experience and partnerships between service providers.
- Allows for psychiatry to adopt a more consultative role.
- Allows for nursing staff to operate as a “pivot” role and to bridge the two clinics by triaging to appropriate services, providing psychoeducational counselling and interim care for monitoring purposes.
- Inter-professional collaboration inherently contributes to professional development (e.g., improved medication treatment competency among family physicians and expanded nursing role in mental health.
- The combined service delivery changes resulted in an 80 per cent reduction in the number of students waiting for mental health services following intake.